Recently, knowledge about the importance of human interaction with microorganisms is questioning the lifestyle of many societies while recognizing the importance of biodiversity in every way.
We had the pleasure of talking to Dr. Clelia Peano, a researcher of the Institute of Genetic and Biomedical Research CNR and Head of Genomic Unit at Humanitas Clinical Center in Milan, Italy. Clelia is part of a group of researchers studying the intestinal microbiome with an aim to understand the functions of microorganisms and their impacts on human health.

It is worth mentioning that the importance of the microbiome is recently recognized by the scientific community. Only since the year 2000, the interactions of microorganisms with their host (animals (humans), plants, soil, water) are known to be relevant to the sustainability, balance and overall health of all constituents within the ecosystem.
But now, let’s allow Clelia to explain it to us:
What is the microbiome?
The microbiome is composed of all microorganisms (e.g. bacteria, fungi, etc.) that colonize an environment. It constitutes an ecosystem.
What is the human microbiome and why is it important?
The human microbiome refers to all microorganisms (e.g. bacteria, fungi) that live within our body.
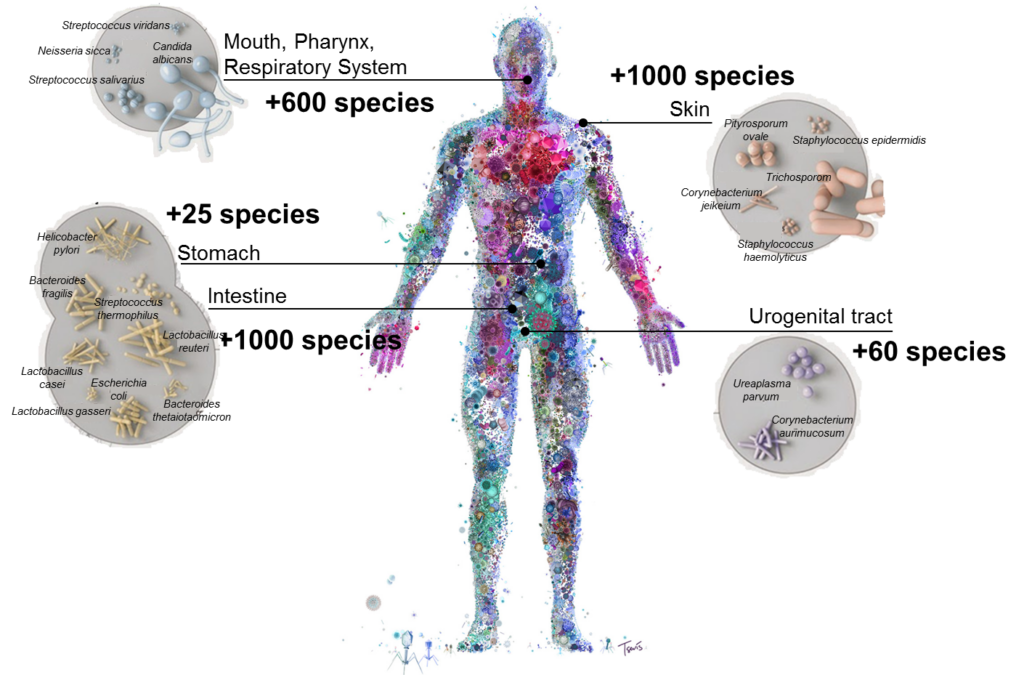
Inside the human body, the skin and the intestine are the organs that are colonized by the largest diversity of bacterial species (more than one thousand species), followed by the oral and pharyngeal tract (more than six hundred spices).
The microbiome is important because our body is dominated by bacteria. As a matter of fact, the bacterial cells colonizing our body are 10 times more abundant than are our human cells.
Inside the intestine, microorganisms exert very important functions such as extracting energy from food, producing vitamins and regulating the immune system, glucose level and metabolism.
How does the microbiome control these body functions?
The microbiome produces metabolites that can contribute to maintain a systemic state of equilibrium or, in some cases, can cause diseases.
The alteration of the correct balance between the microbiome and the immune system is known as dysbiosis, and it can be correlated with the occurrence of diseases such as asthma, diabetes, obesity, liver disease, depression, heart disease, colon cancer and inflammatory bowel disease.
What is the difference between a healthy microbiota and a sick microbiome?
An important difference is related to the relative abundance between different kinds of bacteria. For example, a sick or dysbiotic microbiome has a higher ratio between femicutes/bacteroidetes, and can lead to a systemic inflammation, while a healthy microbiome exhibits a higher bacteroidetes/fermicutes ratio that may be correlated with the maintenance of low levels of inflammation.
What factors influence the microbiome composition?
First of all, the microbiome is an ecosystem that responds and continuously adapts to the organism that hosts it; in this case to our body and lifestyle.
The factors that influence the microbiome composition are:
- food: a diet poor in fiber, high amounts of processed foods and high levels of sugars, predisposes to gut microbiome dysbiosis;
- lifestyle: poor physical activity and excessive/use of drugs can compromise the balance of our microbiome. For example, excessive use of opioids can slow down the digestive process, antipsychotics can have a direct antibacterial effect, gastroprotectors can cause gastric cancer;
- genetic predisposition: our genes play an important role in shaping our intestinal microbiome, this was demonstrated in a study in which from the analysis of 416 pairs of twins, it was observed that identical twins (homozygotes) have a microbiome more similar to each other than different twins (heterozygous).

Two stories to better understand how the intestinal microbiome evolves and transforms, adapting itself over the course of human lives:
1. Comparison between the intestinal microbiome of Hazda and Italians:
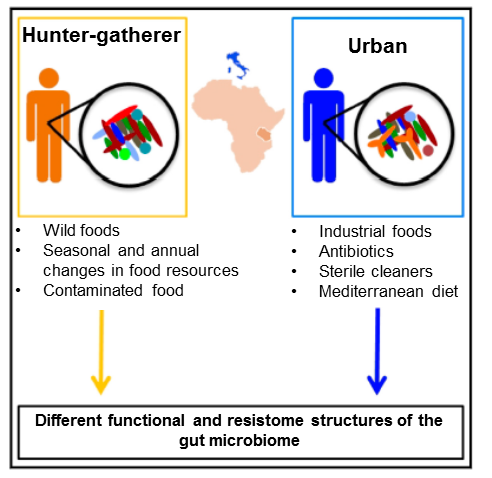
We compared the microbiome of two very different populations: the Hazda, and the Italians.

- The Hadza are a nomadic population living in Africa (Tanzania). They are the last Human hunters and gatherers living on Earth. They have a lifestyle similar to that of the people who lived in the Paleolithic era which occurred more than 10,000 years ago. They have never experienced either agriculture or farming.
- Italians, on the other hand, are a settle/civilized population living in Europe. They have a western lifestyle and live in urbanized environments.
- The Hadza microbiome is dominated by bacteria that serve to degrade fibers while the microbiome of Italians is specialized in the degradation of carbohydrates. Since the diets of these two peoples have a very different composition, the diet of the Hadza is much more diversified and involves the consumption of large quantities of fiber and protein, while the diet of Italians is made up of more than 50% of carbohydrates.
- In the Hadza microbiome, there are no Bifidobacteria, which are present in the microbiome of all other human beings. Their microbiome is different from that of all other peoples: Africans, Europeans and Americans.
- The Italian Microbiome is rich in bacteria that perform functions to metabolize drugs, antibiotics and pollutants. These functions are totally absent in the Hadza microbiome.
- Genes for antibiotic resistance in the Hadza intestine are derived from soil bacteria, which are antibiotic producers, and give an advantage to them.
- Genes for antibiotic resistance in the intestines of Italians derive from the excessive use of these drugs and are a disadvantage for us.
2.Comparison between the intestinal microbiome of newborns and centenarians:
To understand how the microbiome develops and transforms itself over the course of our life, we compared the microbiome of individuals of very different ages: newborns and centenarians.

- The microbiome of infants is dominated by Bifidobacteria, which are essential for the digestion of oligosaccharides (sugars polymers) contained in breast milk and for the correct development of the immune system.
- The interruption of breastfeeding allows the complete maturation of the intestinal microbiome of the newborn.
- The species and bacterial strains found in the microbiome of newborns derive from the mother’s microbiome. The mother is the main source.
- The microbiome is essential for the correct development of the immune system in newborns.
- The intestinal microbiome of centenarians and ultra-centenarians is different from the microbiome that colonizes human bodies during the rest of life.
- In Centenarians and ultra-centenarians, the microbiome is essential for maintaining the state of health and balance within the immune system. Their microbiome is characterized by the presence of the bacterial genus Christensenellaceae.
What are the advantages of the clinical study of the intestinal microbiome?
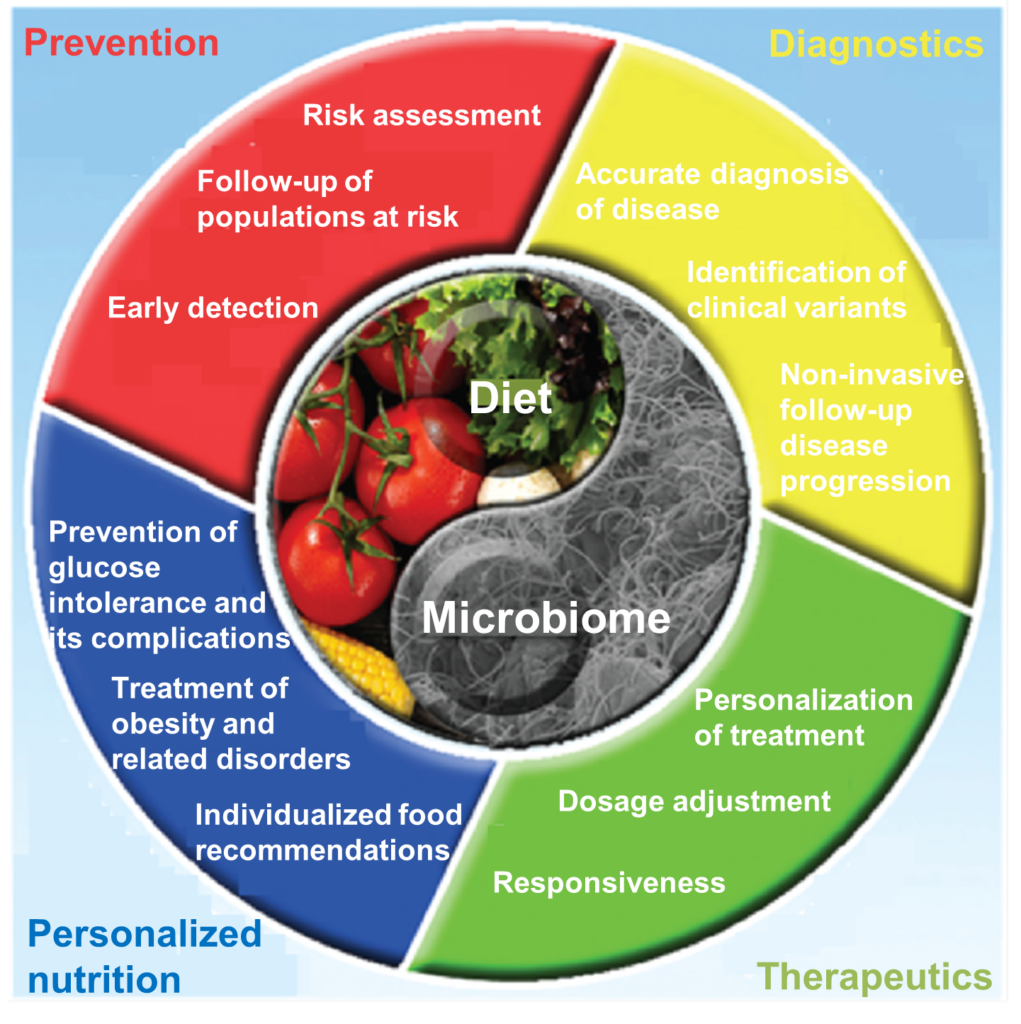
The study of the intestinal microbiome can be fundamental for prevention, early diagnosis and therapy and can help to successfully integrate drug therapies while utilizing a personalized diet.
What awaits us in the future?
Once reliable markers associated with the intestinal microbiome dysbiosis in relation to the onset of pathologies is established and validated, it will be possible to integrate microbiome analysis (from fecal samples) with other non-invasive analysis (urine, blood and saliva samples) to combine different clinical parameters and thus obtain a complete diagnosis that can allow us to identify personalized therapies that include the correct and personalized prescription of drugs and diet.
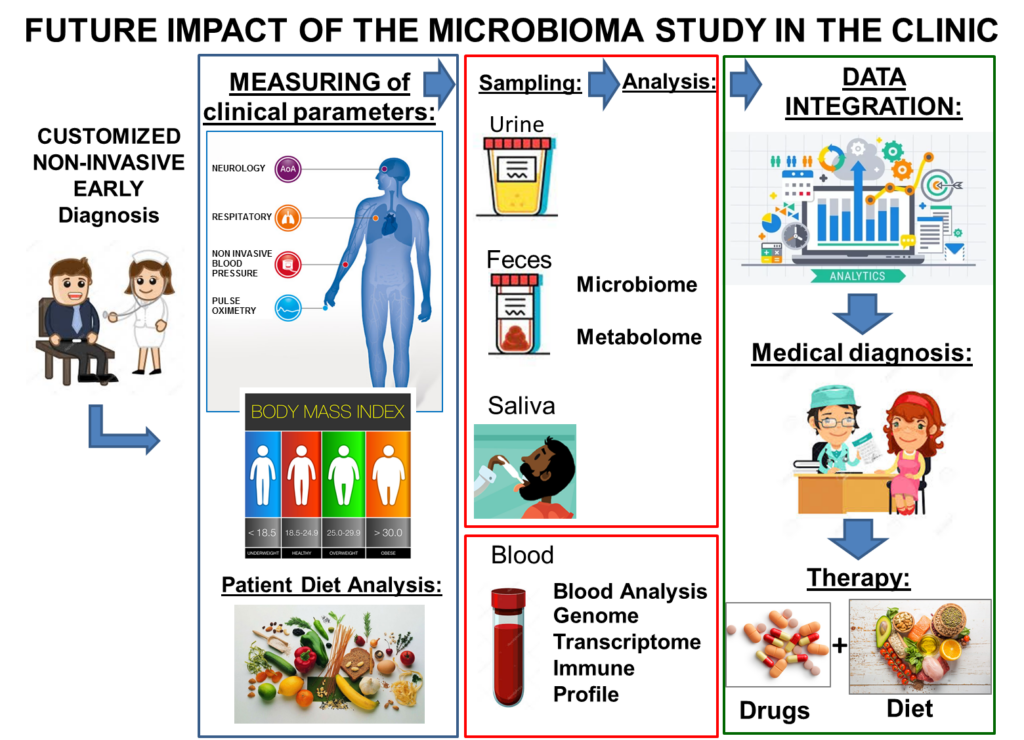
In addition, information about genes and metabolites can help doctors to provide a more effective, comprehensive and personalized health care plan for each individual in the future.
Conclusions:
Our lifestyle (nutrition, exercise, drug intake) affects our health. The quality of the food we eat, the quantity and the diversity in our diet influences the balance of our microbiome and, consequently, our health.
Biodiversity and integration: Biodiversity is always positive both in the environment and within our gut. Let’s respect and improve biodiversity by all means!
Another important point to consider is that the excessive use of antibiotics (in humans, animals and plants) not only affects the microbiome but also causes resistance. Antibiotic resistance is a major problem today! To get an idea, watch this video that illustrates the problem and, for more information, check out the World Health Organization webpage dedicated to this topic. We will develop more on this topic in future posts. Stay tuned!
Publications to which Clelia has made reference:
Nature Communications, 2013. Schnorr, SL. et al. Gut microbiome of the Hadza hunter-gatherers.
Current Biology, 2015. Rampelli, S. et al. Metagenome Sequencing of the Hadza Hunter-Gatherer Gut Microbiota.
Cell, 2014. Goodrich, J.K., et al. Human Genetics Shape the Gut Microbiome.

